Bariatric Surgery FAQs
How long after metabolic and bariatric surgery will I have to be out from work?
After surgery, most patients return to work in one or two weeks. You will have low energy for a while after surgery and may need to have some half days, or work every other day for your first week back. Your surgeon will give you clear instructions. Most jobs want you back in the workplace as soon as possible, even if you can’t perform ALL duties right away. Your safety and the safety of others are extremely important – low energy can be dangerous in some jobs.
Many patients are worried about getting hernias at incisions. That is almost never a problem from work or lifting. Hernias are more often the result of infection. You will not feel well if you do too much.
When can I start exercising again after surgery?
Right away! You will take gentle, short walks even while you are in the hospital. The key is to start slow. Listen to your body and your surgeon. If you lift weights or do sports, stay “low impact” for the first month (avoid competition, think participation). Build slowly over several weeks. If you swim, your wounds need to be healed over before you get back in the water.
Can I have laparoscopic surgery if I have had other abdominal surgery procedures in the past, or have a hernia, or have a stoma?
The general answer to this is yes. Make sure to tell your surgeon and anesthesiologist about all prior operations, especially those on your abdomen and pelvis. Many of us forget childhood operations. It is best to avoid surprises!
Sometimes your surgeon may ask to see the operative report from complicated or unusual procedures, especially those on the esophagus, stomach, or bowels.
Does type 2 diabetes make surgery riskier?
It can. Be sure to follow any instructions from your surgeon about managing your diabetes around the time of surgery. Almost everyone with Type 2 Diabetes sees big improvement or even complete remission after surgery. Some studies have even reported improvement of Type 1 Diabetes after bariatric procedures.
Can I have laparoscopic surgery if I have heart disease?
Yes, but you may need medical clearance from your cardiologist. Bariatric surgery leads to improvement in most problems related to heart disease including:
• High Blood Pressure • Cholesterol • Lipid problems • Heart enlargement (dilated heart, or abnormal thickening) • Vascular (artery and vein) and coronary (heart artery) diseaseDuring the screening process, be sure to let your surgeon or nurse know about any heart conditions you have. Even those with atrial fibrillation, heart valve replacement, or previous stents or heart bypass surgery usually do very well. If you are on blood thinners of any type, expect special instructions just before and after surgery.
When can I get pregnant after metabolic and bariatric surgery? Will the baby be healthy?
Most women are much more fertile after surgery, even with moderate pre-op weight loss. Birth control pills do NOT work as well in heavy patients. Birth control pills are not very reliable during the time your weight is changing. For this reason, having an IUD or using condoms and spermicide with ALL intercourse is needed. Menstrual periods can be very irregular, and you can get pregnant when you least expect it!
Most groups recommend waiting 12-18 months after surgery before getting pregnant.
Many women who become pregnant after surgery are several years older than their friends were when having kids. Being older when pregnant does mean possible increased risks of certain problems. Down’s syndrome and spinal deformities are two examples. The good news is that, after surgery, there is much less risk of experiencing problems during pregnancy (gestational diabetes, eclampsia, macrosomia) and during childbirth. There are also fewer miscarriages and stillbirths than in heavy women who have not had surgery and weight loss.
Kids born after mom’s surgery are LESS at risk of being affected by obesity later, due to activation of certain genes during fetal growth (look up “epigenetics” – for more information). There is also less risk of needing a C section.
Will I need to have plastic surgery? Does insurance pay for plastic surgery?
Most patients have some loose or sagging skin, but it is often more temporary than expected. You will have a lot of change between 6 and 18 months after surgery. Your individual appearance depends upon several things, including how much weight you lose, your age, your genetics and whether or not you exercise or smoke. Generally, loose skin is well-hidden by clothing. Many patients wear compression garments, which can be found online, to help with appearance.
Some patients will choose to have plastic surgery to remove excess skin. Most surgeons recommend waiting at least 18 months, but you can be evaluated before that. Plastic surgery for removal of excess abdominal and breast skin is often covered by insurance for reasons of moisture, hygiene and rash issues.
Arms and other areas may not be covered if they are considered “purely” cosmetic by your insurer. Some of these “less invasive” operations can be done in the clinic, however – so they can be much more affordable!Will I lose my hair after bariatric surgery?
Some hair loss is common between 3 and 6 months following surgery. The reasons for this are not totally understood. Even if you take all recommended supplements, hair loss will be noticed until the follicles come back. Hair loss is almost always temporary. Adequate intake of protein, vitamins and minerals will help to ensure hair re-growth, and avoid longer term thinning.
Will I have to take vitamins and minerals after surgery? Will my insurance pay for these?
You will need to take a multivitamin for life. You may need higher doses of certain vitamins or minerals, especially Iron, Calcium, and Vitamin D. You will also need to have at least yearly lab checks. Insurance almost never pays for vitamin and mineral supplements but usually does pay for labs. You can pay for supplements out of a flex medical account.
If my insurance company will not pay for the surgery, are payment plans available?
There are loan programs available to cover the cost of health expenses such as metabolic and bariatric surgery. Appeals to insurance companies or directly to your employer may reverse a denial of coverage. Metabolic and Bariatric surgery is a health expense that you can deduct from your income tax.
If you are not able to qualify for a loan, the Obesity Action Coalition (OAC) produces a helpful guide titled “Working with Your Insurance Provider – A Guide to Seeking Weight-loss Surgery.” This guide can help you work with your provider and advocate for your surgery to be covered. You can view the OAC guide on their website.
If I am self-pay but I have health insurance, will my insurance company pay the cost of post-operative complications? Complications are often reported under a separate medical billing code. The insurance company may not cover these costs. Appeal is often very helpful, and direct contact with your hospital can make a big difference for final costs. Many surgeons also offer a special insurance policy to cover unexpected additional costs.
Will I have to go on a diet before I have surgery?
Yes. Most bariatric surgeons put their patients on a special pre-operative diet, usually 2 or 3 weeks just before surgery. The reason for the pre-operative diet is to shrink the liver and reduce fat in the abdomen. This helps during the procedure and makes it safer.
Some insurance companies require a physician-monitored diet three to six months prior to surgery as part of their coverage requirement. These diets are very different from the short term diets, and usually are more about food education and showing a willingness to complete appointments and to learn.
Will I have to diet or exercise after the procedure?
No and Yes.
Most people think of a “diet” as a plan that leaves you hungry. That is not the way people feel after surgery. Eventually, most patients get some form of appetite back 6-18 months after surgery. Your appetite is much weaker, and easier to satisfy than before.
This does not mean that you can eat whatever and whenever you want. Healthier food choices are important to best results, but most patients still enjoy tasty food, and even “treats.”
Most patients also think of exercise as something that must be intense and painful (like “boot camp”). Regular, modest activity is far more useful in the long term. Even elite athletes can’t stay at a “peak” every week of the year. Sometimes exercise is work, but if it becomes a punishing, never-ending battle, you will not keep going. Instead, work with your surgeon’s program to find a variety of activities that can work for you. There is no “one-size-fits-all” plan. Expect to learn and change as you go!
For many patients (and normal weight people, too) exercise is more important for regular stress control, and for appetite control, than simply burning off calories. As we age, inactivity can lead to being frail or fragile, which is quite dangerous to overall health. Healthy bones and avoiding muscle loss partly depends on doing weekly weight bearing (including walking) or muscle resistance (weights or similar) exercise.
I am unable to walk.
Almost everyone is able to find some activity to “count” as moderate exercise, even those who are partially paralyzed, or who have arthritis or joint replacement or spine pain. Special therapists may be needed to help find what works for you.
How do I get a letter of necessity?
Some insurance requires this type of letter from either your surgeon or primary care provider before final approval for surgery. Many will just accept your surgeon’s consultation summary note. It is best to ask your insurer directly. Most companies want information pertaining to current weight, height, body mass index, the medical problems related to obesity, your past diet attempt history and why the physician feels it is medically necessary for you to have bariatric surgery. Your bariatric surgeon will often have a sample letter of necessity for you to take to your primary care physician.
Can I go off some of my medications after surgery?
As you lose weight, you may be able to reduce or eliminate the need for many of the medications you take for high blood pressure, heart disease, arthritis, cholesterol, and diabetes. If you have a gastric bypass, sleeve gastrectomy or a duodenal switch, you may even be able to reduce the dosage or discontinue the use of your diabetes medications soon after your procedure.
Online Seminar
After you have viewed the seminar, complete the quiz. Be sure to submit it and include your contact information. Once we receive your results someone from our office will call you. We will review the next step and answer all of your questions.
Upcoming Events
Your Journey Starts Today!
Watch this video and start the process of reclaiming your life!!
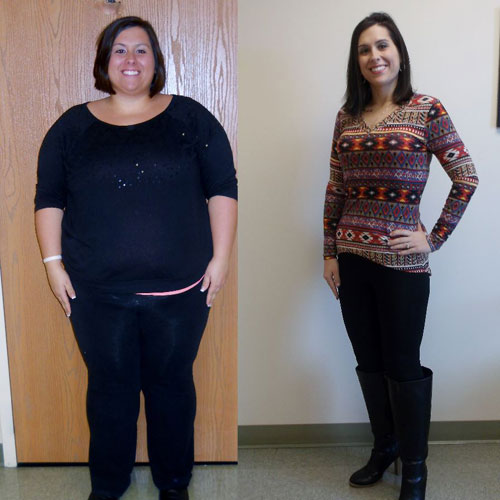
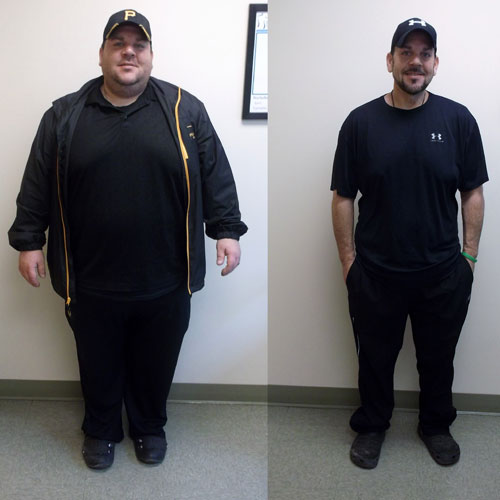
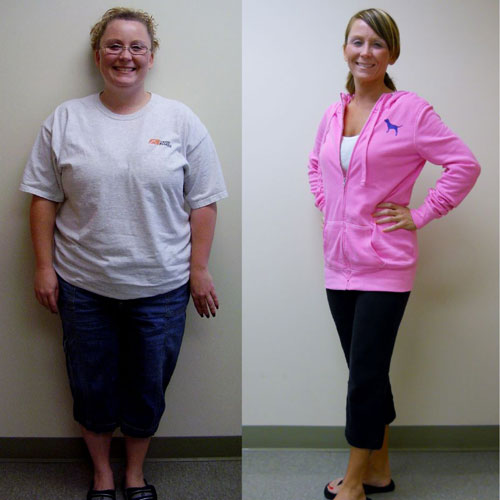
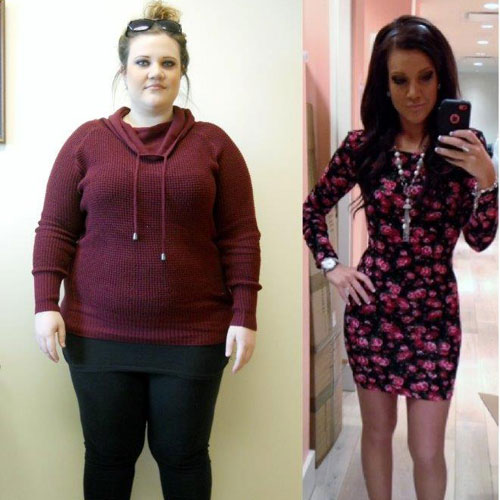
Patient Testimonials
Calculate Your BMI
Bariatric Surgery may be an option.